Aseptic Cleaning, Cleaning & Disinfection, Knowledge Base
Sterile Cleanroom Consumables in GLP-1 Agonist Drug Manufacturing
GLP-1 receptor agonists, such as semaglutide and liraglutide, are produced as sterile injectable medications, making contamination control critical. Any lapse in sterility can have severe consequences for patient safety. For example, in 2024, the FDA investigated a compounding facility after a patient found black particulate matter in a semaglutide vial. The investigation revealed that the facility had used non-sterile ingredients during manufacturing. This incident led the FDA to issue warnings to the facility about the dangers of administering a contaminated drug when the drug is supposed to be sterile.
This incident underscores the crucial importance of strict aseptic manufacturing practices, including the proper use of sterile cleanroom products, in the production of GLP-1 therapies. Moreover, the rising demand for GLP-1 drugs for diabetes and weight loss has increased outsourcing and compounding, which, in turn, heightens regulatory scrutiny of sterility procedures. Authorities emphasize that facilities must follow only strict GMP-compliant processes and use sterile inputs for such injectables. In this context, sterile cleanroom consumables such as lint-free dry wipes, pre-wetted wipes, disinfectants, swabs, mops, gloves, socks, and face masks are essential for maintaining aseptic conditions during the manufacturing of semaglutide, liraglutide, and other GLP-1 analogs.
Cleaning and Disinfection Practices in Aseptic Areas
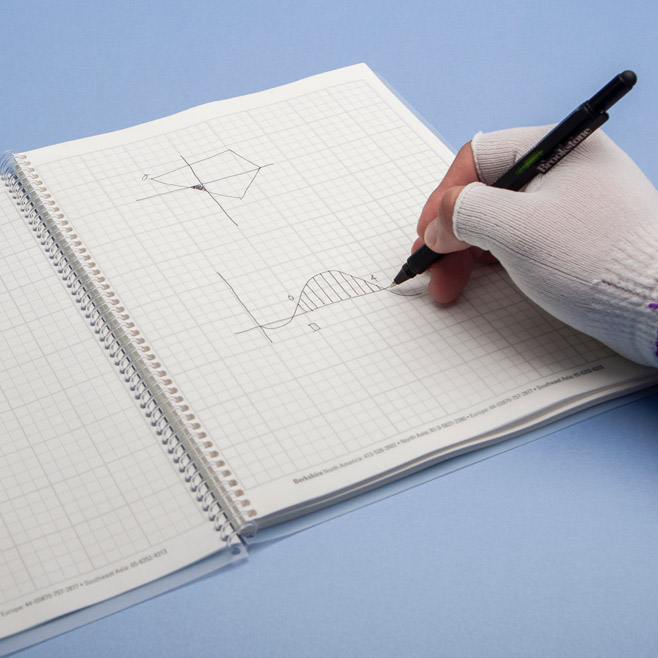
Effective cleaning and disinfection are crucial for maintaining the sterile environment required for manufacturing GLP-1 drugs. The updated EU GMP Annex 1 guidelines stress that cleanrooms must be thoroughly cleaned and regularly disinfected to support contamination control. This includes both chemical disinfection and physical removal of contaminants from surfaces. Sterile wipes, whether dry or pre-wetted, are key consumables in these cleaning procedures. They help ensure that all surfaces, equipment, and components that contact the product are free of particles and microbes before, during, and after production.
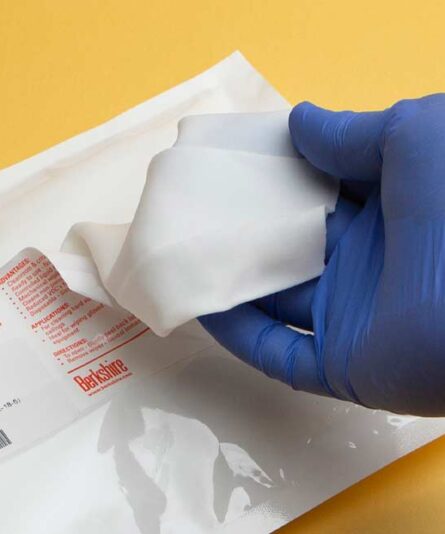
Pre-wetted sterile wipes—soaked in a chemical solution, usually 70% isopropyl alcohol with DI or WFI water—are ready to use straight from the package. For instance, you can use presaturated sterile alcohol wipes to quickly disinfect gloved hands, workbenches, filling machine parts, and other critical surfaces in Grade A/B aseptic zones.
These presaturated wipes deliver a consistent, even wet application to surfaces without needing a separate spraying step. This method not only saves time by reducing the number of items that must be decontaminated or brought into the cleanroom, but also improves surface coverage, lowering the risk of missed spots or insufficient wetting during residue removal. The uniform saturation of each wipe ensures proper contact time for surface sanitization, which is crucial for effectively lowering bioburden. Additionally, removing trigger-spray bottles for each cleaning task can decrease ergonomic strain on workers and reduce the aerosolization of chemicals into the operator’s breathing zone.
In contrast, sterile, dry wipes lack a pre-applied solution, offering greater flexibility in their use. Operators can saturate sterile dry wipes with their chosen cleaning or disinfectant solutions, including sporicidal agents, detergents, and other disinfectants, as specified in the cleaning protocol. This versatility helps apply more potent sporicides or specialized cleaning agents that may not come pre-wetted. For example, you can soak a sterile dry wipe in a sterile hypochlorous acid solution to wipe down surfaces during periodic deep cleaning.
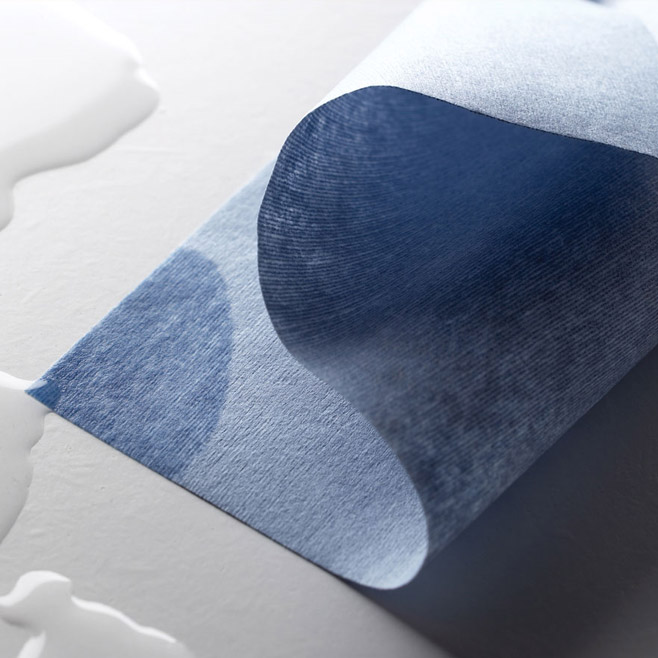
Importantly, both types of wipes are made from low-linting, chemical-resistant materials, such as polyester knits or polyester nonwoven blends, that can withstand exposure to common cleanroom disinfectants without shedding fibers or degrading either the wipes or the chemistry. These wipe materials are compatible with 70% isopropyl alcohol, quaternary ammonium compounds, chlorine-based disinfectants, and peroxides, ensuring that no residues or particles remain after use. Using non-shedding wipes is crucial to prevent fibers or particulates from contaminating critical production areas during cleaning.
Another advantage of using sterile wipes for cleaning is their effectiveness at removing residues. Wiping is a physical action that removes dirt, dust, and residues more effectively than spraying alone. Industry guidance now emphasizes applying disinfectants only after wiping away any visible contaminants or residues to ensure efficacy.
In practice, operators often follow a two-step cleaning process: first wiping down surfaces with a sterile wipe (either dry or moistened with a cleaning solution) to remove spills, powders, or residues, followed by the application of a disinfectant. This approach ensures that disinfectant chemicals can contact the surface directly without interference from films or debris.
Indeed, the revisions to EU Annex 1 explicitly recommend “wiping before disinfecting,” meaning physically cleaning the surface before applying a disinfectant. Sterile wipes facilitate this process and, when used with appropriate cleaning agents, prepare surfaces for effective disinfection.
As summarized in Annex 1, “Contaminants should now be removed before performing disinfection. Sterile wipes can be used for this task.” By eliminating soils and disinfectant residues, wipes help sporicidal agents target microorganisms on surfaces more effectively. This practice is especially critical in facilities producing injectable biologics like semaglutide, where any residue could potentially inactivate sporicides or harbor contaminants if not removed.
Crucially, all wipes used in aseptic processing areas (Grade A/B) are sterilized and validated for use in cleanrooms. A standard method is gamma irradiation, which sterilizes cleanroom wipes, achieving a Sterility Assurance Level (SAL) of 10^−6—meaning a one-in-a-million chance of a viable microorganism. Wipes are usually packaged in double- or triple-layered packaging, enabling an operator to aseptically transfer them into higher-grade areas without compromising sterility.
Using sterile, gamma-irradiated wipes guarantees that the cleaning process does not introduce microbial contamination, which is vital when cleaning surfaces that will come into direct or indirect contact with an injectable drug product. Many cleanroom wipe products include certificates of sterility and low endotoxin levels (pyrogens), since pyrogen contamination poses an additional risk for injectables. By choosing wipes that are certified as both sterile and low-linting, manufacturers of GLP-1 agonists can ensure their cleaning practices do not introduce particles, microbes, or pyrogens.
The frequency of routine cleaning with wipes is an important operational consideration. In active compounding or sterile manufacturing of injectables, critical surfaces are typically wiped down at regular intervals during operations and immediately after interventions or spills. This frequent use of sterile wipes on equipment and gloved hands helps maintain sterility throughout the production process. Since the wipes are single-use and disposable, there is no need to reuse cloths that could potentially redeposit contaminants. Overall, incorporating sterile, dry, and presaturated wipes into the cleaning and disinfection program ensures thorough, consistent, and compliant sanitization of the cleanroom environment.
Maintaining Contamination Control and Aseptic Conditions
In addition to routine cleaning, sterile consumables are essential to the facility’s comprehensive Contamination Control Strategy (CCS). Both FDA and EU regulators expect manufacturers to take a holistic approach to reducing contamination risks at every stage of sterile drug production. The EU’s Annex 1, revised in 2022, specifically requires manufacturers to implement a formal CCS program that covers all critical control points for maintaining sterility, including environmental cleaning and the transfer of materials within the facility.
Sterile wipes are crucial for this strategy because they help control one of the primary sources of contamination: surfaces and equipment in the cleanroom. Using sterile, validated cleaning supplies helps prevent contamination during cleaning. This step is vital because using improper wiping materials or mops has historically posed a significant contamination risk. Regulatory guidelines, both explicitly and implicitly, require the use of appropriate-grade cleaning materials for each cleanroom zone. In high-grade zones (Grades A and B), which correspond to ISO Class 5 environments where open products or sterile components are exposed, all materials introduced must be sterile or properly sanitized. This requirement goes beyond product-contact equipment to include incidental items such as wipes, gloves, garment fabrics, and other materials that could shed particles or microbes.
The FDA’s guidance on aseptic manufacturing and the EU GMP highlight that cleaning processes must not contaminate the environment. Using lint-free, sterile wipes meets these standards by preventing particle shedding and microbial contamination during cleaning. Modern cleanroom wipes, such as polyester microfiber wipes, are designed to release almost no lint and are often ultrasonically or laser-cut with sealed edges to stop fibers from fraying or breaking free. Additionally, these wipes are chemically compatible with the full range of disinfectants and sporicides used in GMP facilities, ensuring they do not interfere with their effectiveness. For example, polyester knit wipes do not absorb or neutralize ethanol or hypochlorous acid in a way that could diminish their effectiveness, which is crucial for maintaining surface disinfection.
Another key aspect of contamination control is reducing residues and ensuring disinfectants work effectively. Sterile wipes help remove residues that could block sporicidal action. Annex 1 now requires that disinfectant programs include a step to eliminate disinfectant residues, as these can create films that trap microbes or hinder sterilants. Wiping with appropriate materials is the most practical way to do this, especially on surfaces such as stainless steel tanks, filling lines, or isolator walls. Facilities that produce GLP-1 agonists in isolators or Restricted Access Barrier Systems (RABS) depend heavily on sterile wipes to decontaminate the interior surfaces of these enclosures. For example, the Berkshire ICT tool enables wipes to be attached for reaching tight crevices inside isolators, demonstrating how wipes are incorporated into contamination control methods and systems for advanced sterile environments.
Cleanroom classifications Grades A through D define the required cleanliness levels and set standards for cleaning consumables. In Grade A/B aseptic areas, only sterile, high-quality wipes are used, often in small, sterile packs that pass through material airlocks. These wipes must meet the strictest standards for particle release and bioburden. In Grade C and D clean areas, which are seen as less critical environments (e.g., formulation or wash/preparation areas), regulations are somewhat more relaxed. Non-sterile cleanroom wipes may be permitted for specific cleaning tasks, provided they are cleanroom-grade (low lint) and their use does not compromise the environment’s cleanliness. Nevertheless, many manufacturers prefer to use sterile wipes throughout all cleanroom grades as a best practice. This approach helps ensure that when items or personnel move from a lower-grade area to a higher-grade area, they are less likely to carry residual contamination and trigger a shutdown.
Cost and practicality are also key considerations. For non-critical cleaning tasks, such as cleaning floors or corridors in Grade D, consider using non-sterile, cleanroom-compatible wipes. The choice of which type to use is usually based on risk and documented in the contamination control plan. Critical surfaces that could directly or indirectly impact the sterile product—such as equipment parts, formulation vessels, and fill room surfaces—are generally cleaned with sterile wipes, even in Grade C environments, especially if there is any risk of product exposure or material transfer to higher-grade areas.
It’s important to consider how wipes fit into disinfectant rotation schemes, which are crucial for contamination control. Good Manufacturing Practice (GMP) guidelines, including those from the FDA and EMA, require facilities to use multiple types of disinfecting agents and to incorporate a sporicide into their cleaning routines periodically. Sterile dry wipes and prewetted wipes play a key role in this process by delivering the selected disinfectant.
For example, a facility might alternate between a quaternary ammonium disinfectant and 70% isopropyl alcohol (IPA) for routine cleaning and schedule a weekly treatment with a sporicidal agent, such as hydrogen peroxide or peracetic acid. Sterile wipes are compatible with all these agents, allowing operators to use pre-saturated quaternary ammonium wipes one day and sterile, dry wipes soaked in sporicide the next. The wipe substrate remains stable and effective with each chemical, ensuring proper application without introducing contaminants or losing fibers. This compatibility makes wipes an essential tool in contamination control.
From a regulatory and GMP perspective, the use of sterile wipes meets expectations for risk management in sterile manufacturing. Current Good Manufacturing Practice (cGMP) regulations require manufacturers to have proper procedures and controls to prevent contamination. For example, FDA regulations (21 CFR 211.42 and 211.113) mandate adequate aseptic processes and facility cleaning. While these regulations do not specify exact consumables, inspectors often check that companies use suitable, validated cleaning materials in aseptic areas as part of their contamination control measures.
Having a documented cleaning program—detailing specific tools such as sterile wipes and mops—is now considered essential. In the production of products like semaglutide and liraglutide, regulatory oversight is rigorous due to their popularity and the risks posed by compromised sterility. The FDA has recently advised both compounding pharmacies and manufacturers that they must use only sterile ingredients and components for sterile injectable drugs, following incidents where some producers failed to adhere to this principle. This requirement applies even to seemingly minor components, including wipes and cleaning fluids.
A comprehensive contamination control program for a GLP-1 agonist production line must clearly define cleaning procedures, the types of wipes used, their sterilization methods, and their storage and handling to ensure they remain sterile until use. During audits or inspections, companies must demonstrate that these consumables meet quality standards and do not present a contamination risk.
In summary, sterile, dry wipes and sterile, presaturated wipes are essential for cleaning, disinfection, and contamination control during the manufacturing of GLP-1 receptor agonist drugs. These wipes help maintain aseptic conditions by enabling thorough cleaning of surfaces and equipment, and they offer a convenient way to apply disinfectants or sporicides. They are used appropriately across various cleanroom grades based on the associated risk.
By incorporating these wipes into standard operating procedures, in accordance with EMA Annex 1 and FDA cGMP guidelines, manufacturers can significantly reduce bioburden and particulate levels in the environment. Alongside other sterile consumables such as gloves, garments, and filters, sterile wipers help ensure the production of high-purity injectable products, such as semaglutide and liraglutide, while maintaining strict contamination control and protecting product quality and patient safety.

























HAVE AN IDEA FOR CONTENT?
We are always looking for ideas and topics to write about.
Contact Us