3D Printing, Bio-Technology, Cleanroom News
How the Humble Inkjet Printer is the New Go-To in Organ Transplantation
From the perfect Super Venti Flat White (yes, it is ‘a thing’) crafted for us at the Starbucks drive-thru to the tailored Tesla designed to indulge our most whimsical aesthetic consideration, the world is becoming increasingly customized whether we like it or not. And however we perceive this transition – good, bad, or indifferent – it is a sufficiently interesting and prevalent phenomenon that we have addressed it on multiple occasions in our pieces about personalizing the allograft and the transgenic technology of cloning. But one aspect of increased personalization we have not yet touched upon is how some technologies are simultaneously promoting and resisting customization. One area in which this is very clear is that of the bio-medical industry. Inasmuch as we marvel at the research that brings us prosthetics with integrated nerve detectors to allow the user to control a limb with their mind or the treatments that use pharmacogenomics to revolutionize individual patient care, we also recognize that certain sectors of the bio-med industry necessarily shun personalization in favor of ‘one fits all’ approach. Which area are we talking about? Counter-intuitive as this might sound, it’s in the realm of organ transplantation. Let’s investigate…
As a species, it has to be admitted – without unnecessary ego – that we humans are a comparatively creative bunch. From art and literature to science and technology, as individuals and as societies we derive our greatest fulfillment from the act of creation, whether in the ethereal realm of philosophy or the real world application of engineering and mechanics. Composing a symphony or building a base on Mars, the drive to bring something new to the world, something that did not exist before we ourselves created it, is inescapable. And it’s an impulse that has been with us seemingly forever. Even a quick glance into the past reminds us that we’ve moved from the cottage industry model of the agrarian era in which crafters/workers painstakingly created one of a kind items by hand to the large scale manufacturing of the Industrial Age. Despite our best efforts – and those of marketing teams everywhere – the hope of feeding the world’s perpetually ballooning population and the tantalizing promise of reaching nirvana through consumerism has not born fruit. Despite sacrificing the custom to the generic, we still do not have the means to feed the global population. And similarly, contrary to the message of every network advertisement, neither personal fulfillment nor world peace are to be purchased via credit card.
And maybe this realization is, in part, behind the recent renaissance in interest in customized, personalized, and handcrafted items. Perhaps it’s a creeping disappointment at the reality of the soulless, identically mass-produced goods whose race-to-the-bottom economics virtually guarantees both environmental degradation and human alienation from the means of production and the products themselves that propels us into another age. An age of anthropocentric personalization – and one where the word truly means situating the individual at the epicenter of the transaction.
Arguably, the alienation between the consumer and the product is nowhere more evident than in the field of replacement body part manufacturing. Although a new hip joint or a prosthetic limb can be a life-saver to patients, the fact remains that all too often the consumer must adapt to the product, not vice versa. And if, in the case of organ transplant or bone replacement, the patient is forced to adopt a diet of pharmaceuticals to ensure that the body does not reject the new part, so be it. It’s the cost of doing business.
Until now.
Facing a lifetime of dialysis, Luke Massella was only 10 years old when surgeons used a piece of his failing bladder tissue to grow another organ for him under laboratory conditions
In an article published by the BBC, journalist Padraig Belton presents an update on a young spina bifida patient whose bladder malfunction led swiftly to kidney failure.(1) Facing a lifetime of dialysis, Luke Massella was only 10 years old when surgeons used a piece of his failing bladder tissue to grow another organ for him under laboratory conditions. After a 2-month grow time, the new bio-identical bladder was implanted into Luke by Dr. Anthony Atala of the Boston Children’s Hospital in Massachusetts in the same sort of procedure that would be used for any other organ transplant. But the difference with this one was that, given the bladder was genetically crafted from Luke’s own cells, the risk of organ rejection was non-existent.
And how did the medical team craft this organ?
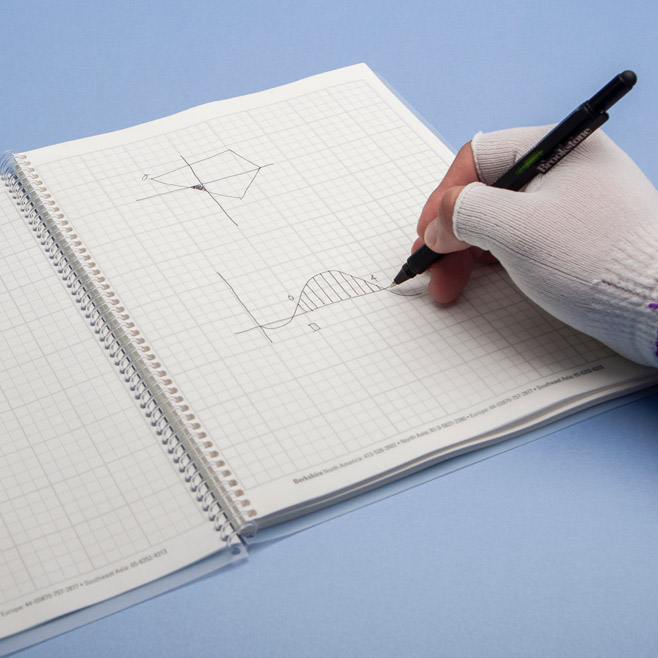
Additive manufacturing – aka 3D printing. Speaking with Belton, Atala, who immigrated to the US from Peru and is now the director of the Wake Forest Institute for Regenerative Medicine in North Carolina, explained that hacking a 3D inkjet printer allowed him to create not only flat tissues such as skin but also tubular structures for the vascular system, along with hollow organs such as the bladder.
The printer, guided by computer imaging, drips cells, layer by layer, over the 3-D scaffold, and the inert mold comes to life.
But the question arises as to how far Atala’s research is different from previous work? The answer to this is ‘in pretty much every significant way…’ Regenerative medicine of this kind blows away the old constraints and restrictions when combined with the technological power of additive manufacturing. Having discovered a new class of stem cells in amniotic fluid, Atala leveraged them to build a variety of body parts – from Luke’s replacement bladder to heart valves, tracheas, livers, and even vaginas which he has successfully transplanted into four female patients. And the device most critical to these transplants? A very ordinary-looking desktop printer. Indeed, in Atala’s two TED Talks, his desktop printer is fêted as the evening’s very special guest star. The surgeon stumbled upon the concept of using ‘a printer cartridge loaded with human cells rather than ink, and a 3-D kidney-shaped substrate of collagen instead of paper. The printer, guided by computer imaging, drips cells, layer by layer, over the 3-D scaffold, and the inert mold comes to life. Over time, millions of cells begin to communicate and function as one organ.’(2) And so a new procedure was born.
And this procedure is based upon the use of a few of the patient’s own cells, harvested via a simple blood draw – an additional distinction of Atala’s process. In the past, the use of stem cells has been limited to those derived from embryonic material, and this resource was, of course, not without controversy. Embryonic stem cells – or ESCs – are derived from cells found in a human blastula, a fertilized egg of around 100 cells in size that has not yet implanted into the uterus. Without implantation, a blastula has a very short viability and those used in research environments are typically cultivated in vitro for highly specific purposes. However, those against ESC research found their opposition on the belief that the blastula represents the first stage of a human being that, inherently, deserves protection. Since it can, subject to a successful implant, eventually become a fetus, the blastula is considered ‘alive’ and those against the use of ESCs in research consider their manipulation to be tantamount to human experimentation.
…any body cell – whether it came from a patient’s blood or fat – could be reprogrammed to become an ‘Induced Pluripotent Stem Cell,’ or iPS cell.
However the use of a patient’s own reprogrammed cells bypasses these ethical considerations. In a process termed ‘differentiation,’ Nobel Prize-winning stem cell researcher Shinya Yamanaka discovered that any body cell – whether it came from a patient’s blood or fat – could be reprogrammed to become an ‘Induced Pluripotent Stem Cell,’ or iPS cell. These cells are exciting insofar as they can divide or renew themselves, at the point of reprogramming they are ‘unspecialized’ blank slates, and they can be customized to become tissue- or organ-specific cells with specialized functions. And, of course, they can be used in great number to create replacement organs. So let’s take a look at how this works.
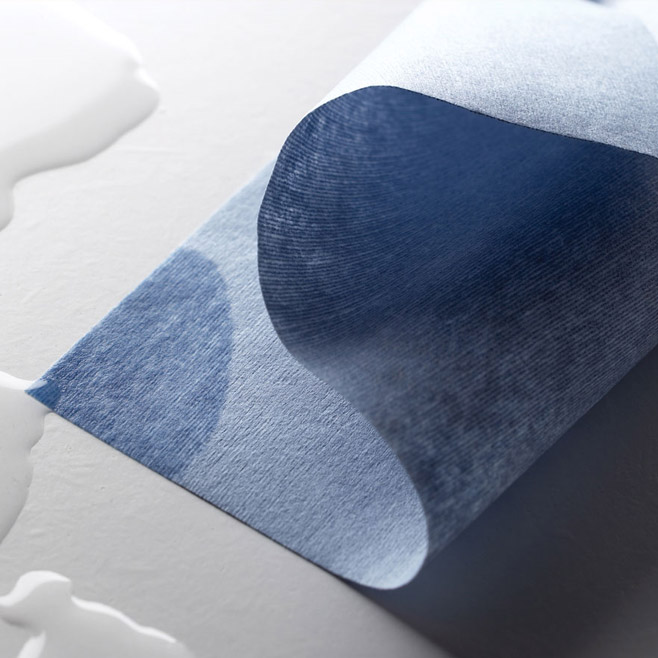
According to BioLife4D, a biotech company based in Buffalo Grove, IL, a simple blood draw harvests cells that are first reprogrammed for conversion to a specialized cell – let’s assume cardiomyocytes, or heart cells.(3) The new heart cells are combined with nutrients to promote growth and are sustained within a hydrogel solution – the ‘bioink’ of the additive process. And at this point anyone familiar with a 3D printer – or indeed with replacing print cartridges for a normal desktop printer – will find themselves scratching their head at the apparent simplicity of the model. Filling ‘ink cartridges’ with the bio-ink, the 3D printer uses a model created from a patient’s MRI scan to deposit drops of ‘ink’ onto a biocompatible and biodegradable scaffold that supports the cells and holds them in formation. Layer by layer and line by line, the bio-ink is laid down on the substrate until a whole organ is created. Moving it to a bioreactor, BioLife4D claims that the organ’s individual cells begin the process of self-organizing, forming networks of tissue that, in time, begin to beat. Once the replacement heart is sufficiently mature and stable, it can be transplanted into the recipient – a precise genetic match and also a perfect fit.
Intelligent printheads are exchangeable by the user to allow for a wide variety of bioinks to be used in crafting skin, heart tissue, bone, or cartilage.
But will any old printer work for this process? Apparently so, if Atala’s successes are anything to judge by, but the days of hacking the departmental inkjet are now – thankfully – long behind us. Cellink, a company with a mission to leverage disruptive technology with the aim of printing not only replacement tissues and organs but also functional cancerous tumors to use in the development of advanced treatment protocols, has released the BIO X bioprinter, as a standalone unit.(4) With a form factor reminiscent of a high end espresso brewing station, the BIO X is interfaced via a large touchscreen that keeps the user firmly in control. Intelligent printheads are exchangeable by the user to allow for a wide variety of bioinks to be used in crafting skin, heart tissue, bone, or cartilage. And, perhaps most critically, the unit also incorporates a patented Clean Chamber Technology that incorporates an aseptic printing area via dual HEPA filters in a positive air pressure chamber environment. Crucially, Cellink boasts that their UV-C germicidal control guarantees the ‘uncompromised sterility’ of the unit.(5)
And contamination control is a very real concern and one that should be a preoccupation for all industry leaders within this technology silo. Why? Do you remember Luke – the 10-year old boy who endured 15 surgeries for spina bifida-related complications? Receiving the healthy, functioning, 3D printed bladder from Dr. Atala changed the course of his life. Within seven years he was captaining his high school wrestling team, he graduated college, and now – as a healthy 27-year old – works as an events organizer. A combination of cutting edge technology and excellence in contamination control created this success. And both of these aspects must go hand in hand as the technology becomes more widely adopted, as all forecasts predict it will. In fact, according to a paper published by Elizabeth Kelly in the University of Pennsylvania Law Review, the market for 3D printed organs – already in the millions of dollars – is growing at an annual rate of 54%, putting market value estimates ‘in the billions within five years.’(6)
So what are the concerns that explain the delay in mainstreaming this technology?
The answer to that question is not easy to pinpoint but one issue is that the regulatory authorities such as the U.S. Food and Drug Administration (FDA) are dragging their collective feet. According to Professor Steven S. Saliterman of the University of Minnesota, the FDA released draft guidance to medical device manufacturers working with additive manufacturing in May 2016 but these guidelines did not address the development of cellular or tissue-based products.(7) Moreover, products derived from stem cells are considered to be somatic cellular therapies and hence are regulated as ‘biologics’ under a section of the Public Health Act, although the jury is still out on whether they should be considered as products, drugs, devices, or a whole other category of item.
And let’s not forget that old fly in the ointment – NOTA.
In 1984, the National Organ Transplant Act (NOTA) was drawn up with the intention of expressly prohibiting the sale of human organs on the open market. Conceived as a way to protect economically exploitable people from the pressure to relinquish a healthy and otherwise personally cherished organ for financial gain, NOTA deems the buying and selling of human organs to be unacceptable. Which, of course, it is. But this otherwise ethically sound piece of legislation in no way foresaw the advent of custom manufactured, bio-identical organs. In the case of tissues created via the additive manufacturing from the patient’s own cells, any question of exploitation for economic gain is moot and, for technologies to flourish and mature, the need for remuneration for services rendered is all too critical. As Elizabeth Kelly summarizes:
‘This is not a question of one person having the power to buy someone else’s life, but rather the idea that a patient may pay to use a part of his or her own body to, with the help of technology, heal. None of the ethical or human rights concerns associated with NOTA’s prohibition are present when organ transplants come from a printer.
In sum, neither the plain text of NOTA nor its legislative history suggests that this law is meant to prohibit the introduction and use of 3D-printed organs to save lives in contemporary society.’(8)
And saving lives is the drive behind this leading edge technology. According to figures from the United Network for Organ Sharing (UNOS), a non-profit that manages the nation’s organ transplant system for the federal government, over 95,000 individuals are currently waiting for a kidney transplant. Almost 14,000 are waiting for a new liver.(9) And the number of donated organs is just a fraction of the number needed. With 20 people dying each day while waiting on the list and a new name being added to it every 10 minutes, the need for a new source of organ harvesting is abundantly clear. So it’s time to mainstream this additive technology and the first step along that path is a new and revised consensus on the legal definition of ‘human organ.’ This consensus will pave the way for the organs or tissues themselves to be defined for regulation ‘as drugs, medical devices, biologics, or any combination of the three,’ all of which fall under the auspices of the FDA.(10) And in falling under the regulatory oversight of this authority, the processes, protocols, and finished ‘products’ would be subject to a multi-tiered set of regulations, thereby ensuring organ/tissue and patient safety.
At least that would seem to be the plan. But at this stage in the technology’s development we can only wait and see how the narrative continues to take shape.
Additive manufacturing of human organs – do you have confidence in the process? What are our biggest areas of concern in this new technology? We’d love to know your thoughts!
References:
- https://www.bbc.com/news/business-45470799
- http://discovermagazine.com/2015/march/13-the-doctor-and-the-salamander
- https://biolife4d.com/process/
- https://cellink.com/about-us/
- https://www.dropbox.com/s/6mzx4rhgocdctc6/BROCHURE%2028%20july%2C%20for%20computer%20view.pdf
- https://scholarship.law.upenn.edu/cgi/viewcontent.cgi?article=9610
- https://saliterman.dl.umn.edu/sites/g/files/…/f/…/bioprinting_-_regulatory_oversight.pdf
- https://scholarship.law.upenn.edu/cgi/viewcontent.cgi?article=9610
- https://unos.org/data/transplant-trends/waiting-list-candidates-by-organ-type/
- https://scholarship.law.upenn.edu/cgi/viewcontent.cgi?article=9610




















Pingback: Healthcare Innovations: Going Too Far or Not Far Enough? – Radio Free
Pingback: Printing Human Organs: Additive Manufacturing in Healthcare
Pingback: A future with sustainable physical music media - info24.news