Cleanroom News
COVID versus Camelid: Do Nanobodies Do a Body Good?
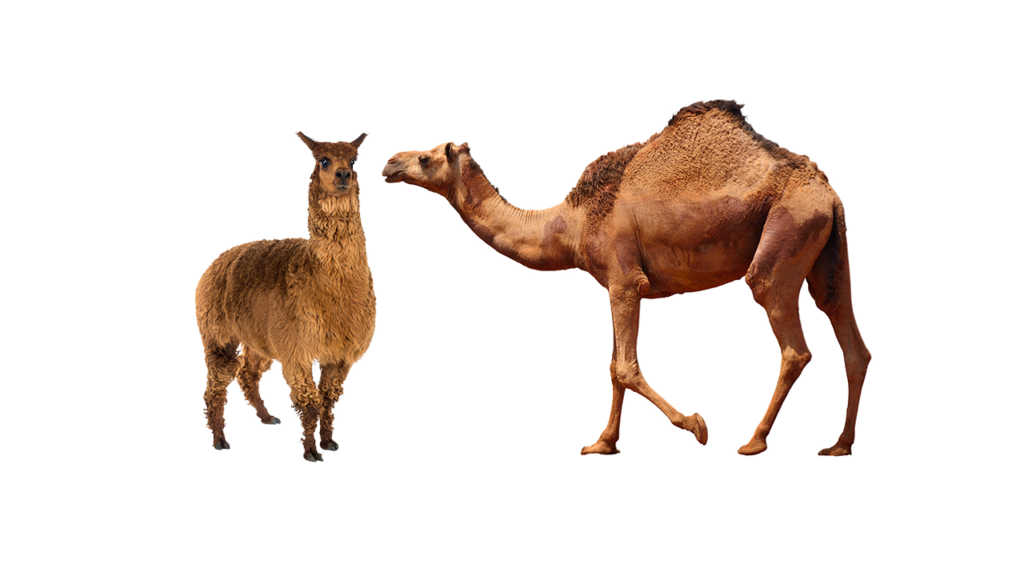
Very occasionally a story emerges that stops us in our tracks and gives us pause for reflection. This year has seen its fair share of those, it must be admitted, because 2020 has – by anyone’s measure – been quite the year. And so it is again that today’s pandemic ponderings revolves around cleanroom COVID-19 research but this time with a puzzling source of potential protection. When animal test subjects and trials come to mind, we tend to picture rodents in the lab, so would it surprise you if we also mentioned somewhat larger pandemic pioneers? Camelidae – the family that includes alpacas, llamas, and of course camels – may be the newest research test subjects to enter the cleanroom. Not literally, of course, but in terms of their antibodies. Have we piqued your curiosity? Read on to find out more…
The implications of a recently published article in the journal Science are making their way through the research community addressing the spread of COVID-19. Lead author Yufei Xiang of the University of Pittsburgh, PA, and his team set out to engineer a cost-effective and efficient therapy to inhibit viral infection, based in proteomics and immunization. Immunization is, admittedly, not a new tool in the challenge of halting the spread of coronavirus, however the specific nature of Xiang et al’s immunization protocol – the use of camelid antibodies – could definitely be described as novel.
So why place the study’s focus on camels, llamas, and the like?
For an answer to that question, we’ll have to go back to the laboratories of the Free University of Belgium in 1990 where research students attempted to clone antibody cells from hybrid cells of tumors and B-lymphocytes. Initially seeking to develop a test kit to detect the presence of trypanosome infection in water buffaloes, the students discovered that antibodies generated in camels are unique in several ways. Not only possessing an unusual structure, the cells are resistant to heat and acids, which makes them easier to handle without risking damage. Moreover, they are highly soluble, relatively small in size, and contain ‘an HCAb antigen-binding domain that was subsequently named as the VHH domain.’(1) The significance of the VHH resides in its ability to ‘recognize antigens that are as small as 12 to 15 kilodaltons (kDa).’(2) These factors and more led to the university patenting the concept of nanobodies (Nbs) – camelid antibodies just one tenth the size of regular antibody cells – and creating Ablynx, a research entity founded via the university’s tech transfer. Today, the company which was acquired by Sanofi in 2018 is collaborating with other key players in the biopharmaceutical field such as Novartis, P&G Pharmaceuticals, and Wyeth Pharmaceuticals.
So is there more to the current interest in camelid nanobodies than just their miniaturization?
Absolutely. According to Ablynx, nanobodies are ‘proprietary therapeutic proteins based on single-domain antibody fragments, which combine the advantages of conventional antibody drugs with some of the features of small-molecule drugs [and have] potential uses in the treatment of a range of serious and life-threatening human diseases. Ablynx advances a portfolio of Nanobody-based therapeutic programs in several major disease areas, including inflammation, haematology, immuno-oncology and oncology.’(3)
And, it is to be assumed, in the area of COVID-19. How? Let’s take a moment to refresh our collective memory on cellular biology…
Although their specific amino acid sequences vary, all antibody cells are composed of four polypeptides – two heavy chains and two light chains – that are joined together in the shape of a ‘Y.’ The basic job of an antibody is recognizing and neutralizing a pathogen, using its ‘Fab fragment’ – a fragment anti-binding region to connect an invading cell’s epitrope (binding site) much like a lock and key. Cells dubbed ‘monoclonal antibodies’ can be genetically engineered to detect and bind to a particular epitrope on a specific antigen, making them very precise and targeted killers.
According to an article in Cell Chemical Biology, a research journal published by Cell Press, llama antibody cells ‘comprise the antigen binding fragment of the heavy chain of an antibody [and] can be encoded by a single gene and produced in bacteria and yeast for a fifth of the cost of a mAb [monoclonal antibody].’(4) And their ability to perform as a mAb is significant insofar as they mimic that antibody’s customizability. In short, these tiny and less expensive warriors can be engineered to seek out and destroy a specific pathogen – one such as the novel coronavirus, for instance.
So let’s now return to examining the role of llamas in vaccine development – or at least at one specific individual at the University of Pittsburgh called Wally.
The virus SARS-CoV-2, popularly known as COVID-19, enters host cells using a spike protein and begins the process of infection, the end result of which we are now seeing on a global scale. Inoculating Wally with a piece of the virus’ spike protein, the researchers induced infection and used mass spectrometry to identify resulting nanobodies. And they developed within a relatively rapid timeframe, with bloodstream antibodies detected within just two short months of exposure. Subsequent testing revealed promising results: not only had antibodies developed swiftly, but they were also potent. So potent, in fact, that when they came into contact with live coronavirus particles just a fraction of a single nanobody effectively prevented the infection of up to one million host cells.
At a time when individual cases of COVID-19 infections continue to rise seemingly unchecked, hospitals are warning of maxed out capacity, and deaths are approaching a quarter million in the US alone, Wally’s news does seem like news worth celebrating. Especially if we add into the equation work from the University of Texas at Austin where researchers working with cells from Wally’s compatriots have discovered a camelid antibody that neutralizes Severe Acute Respiratory Syndrome (SARS). This virus is, as the name suggests, a close cousin of SARS-CoV-2. We await further developments from the work with Wally and his ilk with great anticipation.
As it currently stands in the frenetic biopharma industry race to develop, test, and profit from a COVID-19 vaccine, the winner may be the one first past the post. But reaching that post involves gaining Food and Drug Administration (FDA) approval through conforming to the full suite of current Good Manufacturing Practices (cGMPs), the adherence to Hazard Analysis and Critical Control Points (HACCP) protocols, and all of the usual regulatory hurdles along the race course. However, what’s not yet being emphasized is another major hurdle: the question of global distribution, which is undoubtedly set to be a political, technical, and logistical nightmare. Here in the US, as in Europe, Australia and New Zealand, and other similar nations, getting a vaccine to those who need it will be a challenge but one which is not insurmountable. However, to effectively end the pandemic, therapeutic interventions must involve wrap-around, wide-scale dissemination of the drug, which necessitates alternative distribution mechanisms. According to an article in Global Biodefense, ‘[the] majority of COVID-19 vaccines under development – like the Moderna and Pfizer vaccines – are new RNA-based vaccines. If they get too warm or too cold they spoil.’(5) The existing protocol is based on the vaccine ‘cold chain’ which demands strict temperature control from manufacture to patient vaccination. However, the article succinctly captures the challenge therein: ‘Ultimately, hundreds of millions of people in the U.S. and billions globally are going to need a coronavirus vaccine – and potentially two doses of it. This mass vaccination effort is going to require a complex vaccine cold chain on a scale like never before. The current vaccine cold chain is not up to the task, and expanding the supply chain is not going to be easy.’(6)
According to Supply Chain Dive, up to a quarter of all vaccine doses are degraded by the time their reach their destination at an estimated cost of $34.1 billion per annum.(7) And, of course, that doesn’t factor in the human cost of receiving ineffective drugs or none at all. But this is where nanobody technology could potentially come to the fore. As already noted, nanobodies are highly thermostable and may be stored, according to the team at the University of Pittsburgh School of Medicine, for anything up to six weeks. Of course, the final shelf life may be longer but at this stage of the R&D cycle we can’t yet be sure. However with perishability as a blocker to widespread vaccination in areas where transport networks are sub-optimal and reliable refrigeration unavailable, a thermostable vaccine would offer serious benefits.
An additional advantage to this new technology might also be the way it is given to the patient. Nanobody-based therapy is radically different insofar as it is administered via the inhalation of an intra-nasal mist, as opposed to an injection.
This has multiple benefits including making possible its administration even in the absence of trained medics and in delivering the antibodies exactly where they are needed – directly to the lungs. Indeed, writing in Science, lead author Yufei Xiang summarizes the benefits of nanobody-based therapeutics thus: ‘Flexible and efficient administration, such as inhalation may further improve their antiviral efficacy while minimizing the dose, cost, and potential toxicity for clinical applications […] These high-quality Nbs can also be applied as rapid and economic point-of-care diagnostics. We envision that the Nb technology described here will contribute to curbing the current pandemic and possibly a future event.’(8)
This is an exciting scenario and, at a time when media cycles are barely keeping pace with the fast-changing world, any good news emerging from the nation’s biopharma cleanrooms and controlled environments is more than welcome.
And the speed with which we are adapting to the myriad challenges and developing solutions to them is testament to the creativity underlying our innovation. Right now, it remains to be seen whether a camelid Nbs vaccine will emerge as the winning therapy, one that quarantines not us but the virus, securing it under layers of biosafety stewardship protocols and relegating it to the annals of biomedical history. But in an otherwise dark time even knowing that multiple approaches are being actively pursued brings the hope we need for a pandemic-free future.
We’d love to know your reactions to this research. Do you think that nanobodies offer the greatest hope for a global vaccine? Or if you have reservations, what are they?
References:
- https://www.news-medical.net/life-sciences/What-are-Camelid-Antibodies.aspx
- ibid
- https://www.ablynx.com/our-company/overview/
- https://www.cell.com/cell-chemical-biology/comments/S1074-5521(06)00433-9
- https://globalbiodefense.com/2020/10/05/the-challenges-of-vaccine-cold-chain-distribution-must-be-met-to-end-the-pandemic/
- ibid
- https://www.supplychaindive.com/news/coronavirus-vaccine-cold-chain-tracking-iot-sensor-technology/583168/
- https://science.sciencemag.org/content/early/2020/11/04/science.abe4747



















Pingback: COVID versus Camelid: Do Nanobodies Do a Body Good? - Cleanroom News | Berkshire Corporation