Cleanrooms
Stay Up To Date: How Much Do You Know About Controlling Gram-Negative Bacteria in a Cleanroom?
From cocci which are round in shape, to bacilli which look like rods, to spirals which are sub-classed according to the number of their twists per cell, microorganisms are fascinating little creatures. At least to those who study them. In structure, the three types are not only differentiated by shape but also by arrangement such as diplo (paired), staphylo (clusters), and strepto (chained), and pleomorphs can assume one of many shapes, dependent – we assume – upon their mood. But neither shape nor arrangement is the subject of today’s examination of the micro world and its challenges to our cleanroom environments. Instead we’re exploring bacteriological gram type – negative and positive – and discussing why excellent environmental hygiene is critically important to managing them.
Today’s focus is specifically on gram-negative bacteria and why it’s important to know as much as possible about them, beginning, of course, with nomenclature. According to Merck, gram-negative bacteria are simply those which turn red when subjected to the Gram staining process. Developed in 1884 by Danish bacteriologist Hans Christian Gram, the process divides bacteria into two basic groups – gram-negative and gram-positive. The process stains bacteria either magenta (‘red’) or crystal violet (often referred to as ‘blue’) due to differences in the structure and composition of their cell walls. Gram initially developed the technique of cell staining when, during the course of his work on lung tissue at a Berlin morgue, he struggled to isolate the bacteria visually.
Whilst very effective, the 4-part process is relatively simple:
- a sample of the bacterial culture is fixed to a slide using heat and then flushed with the primary dye stain – crystal violet
- a trapping agent – iodide – is applied to the sample, binding to the crystal violet within the cell membranes.
At this stage, the gram-negative and gram-positive cultures will be indistinguishable from one another given that they will both be stained purple. However, at stage #3, their difference will become apparent:
- alcohol or acetone is applied to decolorize the sample, resulting in a gram-positive bacterium remaining purple and its gram-negative counterpart becoming colorless
- counterstaining with safranin confirms the status of either bacterium
The color difference within the microorganisms is a result of the decolorizer’s interaction with cellular lipids. In a gram-negative cell, the alcohol/acetone wash flushes out the trapping agent’s coloration as it strips away the endotoxic lipopolysaccharide layer – the outermost membrane – and reveals the inner peptidoglycan layer. (A human-centric analogy would be the removal of the epidermis to reveal the dermis below.) With a gram-positive cell, however, the peptidoglycan is composed of several layers in which the purple color remains trapped. The subsequent application of counterstain color affects both types of bacteria but is effectively hidden by the darker purple of the trapped iodine whilst visible in the colorless gram-negative cell.
So why do the stain color and kind of bacteria matter?
In a clinical setting such as a hospital, it’s critical to be able to identify a bacterium in order to be able to determine the root of an infection. According to the Centers for Disease Control and Prevention (CDC), ‘Gram-negative bacteria cause infections including pneumonia, bloodstream infections, wound or surgical site infections, and meningitis in healthcare settings.’(1) That’s very generalized data, so let’s take a closer look at one specific gram-negative bacterium: Acinetobacter baumannii.
An opportunistic pathogen, acinetobacter is associated with wet environments and is characterized as a ‘strictly aerobic, non-fermenting, non-fastidious, non-motile, catalase-positive, oxidase-negative bacteria.’(2) In a cleanroom setting, stagnant water, substandard plumbing, bad piping hoses, unclean sinks or drains, and poor equipment sanitization give gram-negative bacteria the perfect pied à terre in which to settle, replicate, and thrive. And in a research, development, or manufacturing environment, this can augment the risk of E. Coli, Enterobacter, and biofilms – all too often the precursors of extremely costly product recalls for manufacturers.
Gram-negatives also seek out moisture in a clinical setting, attacking mucous membranes and soft tissues through damage to the protective epidermal layer.
Once established, human tissues infected by these bacteria display a tell-tale ‘orange skin’ appearance which later sprouts clear vesicles or fluid-filled blisters. Tissue necrosis will then occur and, if untreated, the infection can become systemic and result in death.
Furthermore, necrosis is not the only potential outcome of exposure to this gram-negative bacterium. Bloodstream infections are possible, as is meningitis. And in this era of mass hospitalization and intensive use of Intensive Care, Hospital-Acquired Pneumonia – also known as Ventilator-Associated Pneumonia (VAP) – is another potential outcome. Within the context of an on-going pandemic, a potentially fatal bacterial infection associated with critical life support equipment is a truly terrifying prospect.
But we have antibiotics to treat these kinds of infections, don’t we? Yes, but as the CDC goes on to point out, pathogens such as acinetobacter ‘are resistant to multiple drugs and are increasingly resistant to most available antibiotics. These bacteria have built-in abilities to find new ways to be resistant and can pass along genetic materials that allow other bacteria to become drug-resistant as well.’(3) In fact, as Aoife Howard, co-author of the paper ‘Acinetobacter baumannii. An emerging opportunistic pathogen,’ goes on to note, strains of acinetobacter are not only multi- but also pandrug-resistant since ‘upregulation of the organism’s innate resistance mechanisms coupled with the acquisition of foreign determinants have played a crucial role in the express route the organism has taken to becoming a multidrug-resistant pathogen.’(4)
So, in this specific gram-negative bacterium, what we are facing is a virulent type of necrotizing pathogen that can deftly outwit our modern antibiotics and antibacterials. Although indeed true, if we zoom back out again and take a look at the bigger picture, there is nonetheless some cause for optimism. While we know that microorganisms such as gram-negative bacteria are resilient, they are not indestructible. And we know both where they hide and how to eliminate them. Writing for Pharmaceutical Online, Crystal M. Booth notes: ‘Microorganisms are present in most habitats [including] soil, water, plants, animals, hot springs, the deep sea, food, beverages, skin, and hair.’(5) They are easy to spread through the air or via touch contact with surfaces or with other people. It should go without saying that this challenge is faced by healthcare facilities and contamination-controlled environments alike.
So in knowing how to go about eradicating them, understanding the problem is the first step. Booth goes on to say that typically ‘80 to 90 percent of normal microbial flora identified in a cleanroom environment is generated from humans.’(6) And, when inadequate personal hygiene is combined with poor facility maintenance and/or cleaning, the situation is ripe for gram-negative organisms to thrive. Booth continues: ‘When Gram negative rods are recovered in cleanrooms, sources of stagnant water or moisture are usually present. Gram negative bacteria can be found in water systems, on surfaces due to improper disinfection practices, in standing water, in piping or hoses with moisture, and in sinks or drains. […] Poor aseptic technique can contribute to spreading the contamination.’(7)
Of course, it is rarely easy to maintain a completely sterile environment, so if bacterial contamination is discovered, the next line of defense is to ensure proper remediation – and this doesn’t just mean a liberal spritz of disinfectant. Earlier in the article, we discussed bacterial structure and the presence of endotoxins – a class of lipopolysaccharides – within their cellular walls. When a gram-negative bacterium is killed through the use of – for example – quaternary ammonium compounds, pyrogenic (‘fever-inducing’) endotoxins spill out of the ruptured cell, leaving behind a seething mass of toxic waste, albeit on a very small scale. (For more on endotoxins and pyrogens, we have a Knowledge Base article here.)
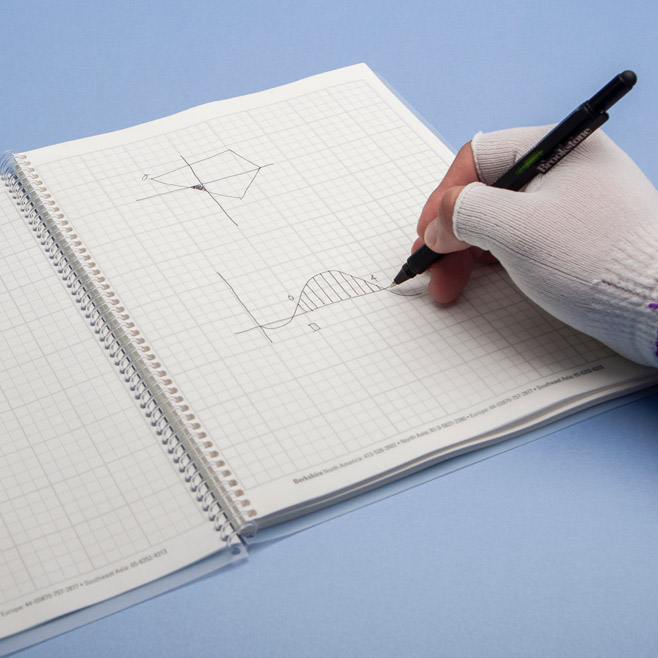
So post-eradication, the toxic remains of the microorganisms must be removed and this is where wipers play a critical role.
Not only do products such as the low endotoxin wipers in the SatPax®, MicroFirst®, and MicroSeal SuperSorb® lines (for example) eliminate bacteria completely, they also clean up after the fact. And our wipers are tested for endotoxin content to ensure that they do not contribute to the problem by adding significant amounts of pyrogens to the freshly wiped surfaces. For those in the healthcare, pharmaceutical, and medical device manufacturing industries, the use of these (and similar Berkshire wipers) offers an effective, Limulus Amebocyte Lysate (LAL)-tested product which conforms to the Food and Drug Administration’s (FDA) test for endotoxins. To learn more about Berkshire’s Low Endotoxin Wipes, click here.
Low Endotoxin Wipes
So where does this leave us? Hopefully with at least a little more clarity on the dangers of gram-negative bacteria both in a healthcare setting and a cleanroom environment. We’re working on a similar discussion of gram-positives for future publication so watch this space for more to come! And in the meantime, if you’ve enjoyed this article consider taking a break from the joy of annihilating work surface bacteria, and let us know your thoughts in the comments!
For all of your Cleanroom Wipe needs visit Berkshire.com!
References:
- https://www.cdc.gov/hai/organisms/gram-negative-bacteria.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3442836/
- https://www.cdc.gov/hai/organisms/gram-negative-bacteria.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3442836/
- https://www.pharmaceuticalonline.com/doc/cleanroom-microbiology-identifying-controlling-sources-of-contamination-0001
- ibid
- ibid



















HAVE AN IDEA FOR CONTENT?
We are always looking for ideas and topics to write about.
Contact Us